-
About
- Departments & Offices
-
Academics
- Public Health
- Biomedical Sciences
- Physician Assistant
- Special Master’s (MBS)
-
Admissions & Financial Aid
- Tuition & Fees
-
Student Experience
-
- Student Resources by Program
- Academic & Student Support
- Wellness & Wellbeing
- Student Life
- Events & Traditions
-
-
Research
- Research Labs & Centers
- Tufts University-Tufts Medicine Research Enterprise
-
Local & Global Engagement
- Global Health Programs
- Community Engagement
Clues about a New Deadly Fungus
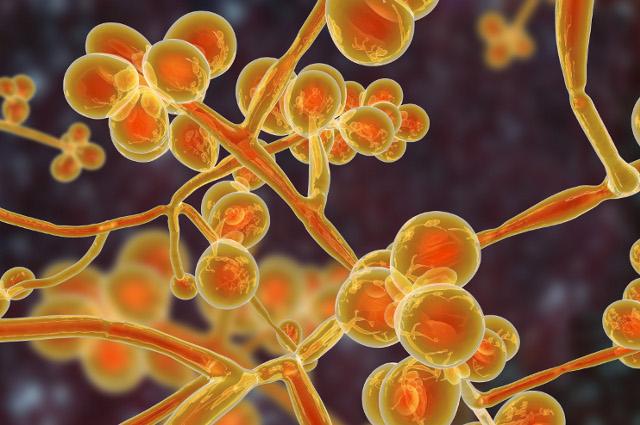
The new fungus Candida auris may seem mysterious but the Kumamoto Lab at Tufts School of Medicine believe they can use what we have learned from studying other fungi to deal with this new and deadly organism.
By Carol A. Kumamoto and Jesus A. Romo
It seems like every few years there’s a virus or bacterium that threatens human health in a new way. But a new fungus that is a threat to humans? That doesn’t happen very often. That’s why we in the medical mycology community—the people who study dangerous fungi—are so intrigued and concerned by news reports about a new, deadly fungus called Candida auris.
C. auris is believed to have been first identified in 2009 in the ear canal of a patient in Japan, but has taken the medical community by surprise with its rapid spread across the globe in the last decade. C. auris has now been detected in about twenty countries and shows no evidence of stopping.
What makes this well-traveled fungus fascinating and scary? Unlike other species of Candida, it is known to survive in hospital rooms for prolonged periods of time and is responsible for several outbreaks due to patient-to-patient transmission. The most concerning characteristic of this fungus, however, is its ability to withstand anti-fungal treatment.
We are a team of medical mycologists working at Tufts and specializing in the study of a different fungus, Candida albicans, and how it affects human health. We have been interested in C. albicans for years because its interactions with humans are so complex—sometimes it seems friendly and sometimes it is our enemy. The new fungus C. auris seems very mysterious, but we believe we can use what we have learned from studying other fungi to deal with this new organism.
A Formidable New Adversary
Fungi are among the most successful, resilient, and fascinating groups of organisms on Earth. In fact, the largest organism on Earth is believed to be a mushroom. We do not know exactly how long fungi have been around, but it is believed that they might be some of the oldest land dwellers on Earth.
During their existence, fungi have dealt with a multitude of global catastrophes, including five—and perhaps a coming sixth—mass extinctions. In order to survive and thrive during these extreme conditions, fungi have developed amazing strategies which have allowed them to conquer every environment imaginable. Out of the estimated 1.5 to 5 million fungal species on Earth, about 300 are able to cause disease in humans. In the case of C. auris, we know whom it is related to, but we do not know where it came from or how people acquire it.
Unlike anti-bacterials, the number of types of useful anti-fungal drugs is quite limited. There are only three main classes, and the chance of discovering new drugs is limited by the fact that fungi are in the group of organisms called eukaryotes, as humans are, which makes it difficult to find a drug that can kill a fungus but not a person. Additionally, anti-fungal resistance has been emerging over the past few decades in some fungi that cause disease in humans, but C. auris’ resistance to anti-fungals leaves other resistant fungi in the dust. Some C. auris strains are resistant to all classes of clinically used anti-fungals, which is extremely alarming.
C. auris is also able to form biofilms, which are microbial communities attached to a surface and protected by a “glue-like” layer. The architecture of the biofilm protects C. auris from anti-fungals and immune system attacks. In the context of health care, microbial biofilms often form on plastics such as catheters, pacemakers and other implanted devices. These biofilms have been well studied for many microbes, but we do not fully understand the importance of biofilms formed by C. auris in the context of human disease.
Where did this new pathogen come from? Why is it highly drug-resistant and able to spread so easily? How does it interact with our body and the other microbes in and on our body? While we don’t know much about C. auris yet, we know quite a bit more about its distant cousin, C. albicans.
Lessons from C. albicans
The fungus C. albicans was first described by Hippocrates in 400 B.C. when he was describing oral thrush, a disease characterized by white lesions that form in the oral cavity when there is overgrowth of C. albicans. Since then, C. albicans has become one of the most studied fungi next to Saccharomyces cerevisiae, the baker’s and brewer’s yeast.
C. albicans can cause fatal infections in humans, but more commonly this fungus resides in the human body, in the gut, or on the skin as a harmless member of the microbiome, which is the whole collection of microorganisms in and on our bodies.
In a study from the 1970s, investigators showed that if you test one-month-old babies for fungi, you find that almost every one of them had acquired a fungus, usually C. albicans. The conclusion was that it is completely normal for a person to have C. albicans in their body.
Yet, if the person develops a weakened immune system, the C. albicans that was already inhabiting their gut could become dangerous by changing its shape to elongated cells known as hyphae. These hyphae are then able to invade and destroy tissue, enter the bloodstream, and cause a potentially fatal infection.
Hope in the Time of C. auris
A few years ago, our group started to wonder why this happens. Why is it OK that humans would have a fungus in our bodies that might kill us if conditions changed? Is there anything that the fungus does that might be good? We decided to investigate this question using a mouse model of infection.
We found that mice that carried C. albicans in their guts were protected from lethal doses of the bacterium Clostridioides difficile (C. diff). These findings showed that C. albicans has wide-ranging effects on its human host, and in some situations could be beneficial.
Many aspects of C. albicans biology have been studied. We have a good understanding of what type of conditions push C. albicans to become a disease-causing organism and form biofilms. We also have identified some of the tricks that allow it to become drug resistant, such as acquiring mutations in a gene called ERG11. Interestingly, the ERG11 gene of C. auris has also acquired mutations that contribute to its drug resistance.
So why is it important to consider C. albicans and other related Candida species when we are dealing with C. auris? If we understand some of the complex ways that C. albicans interacts with humans, this knowledge gives us a window to understand how C. auris might cause disease in people. Additionally, the lessons learned from studying C. albicans and other related fungi could help us develop solutions to deal with C. auris.
Know thy enemy, in this case, by understanding its family.
Carol A. Kumamoto is professor of molecular biology and microbiology at the Tufts School of Medicine. Jesus A. Romo is a postdoctoral fellow in molecular biology and microbiology at the Tufts School of Medicine.
Department:
Molecular Biology and Microbiology