-
About
- Departments & Offices
-
Academics
- Public Health
- Biomedical Sciences
- Physician Assistant
- Special Master’s (MBS)
-
Admissions & Financial Aid
- Tuition & Fees
-
Student Experience
-
- Student Resources by Program
- Academic & Student Support
- Wellness & Wellbeing
- Student Life
- Events & Traditions
-
-
Research
- Research Labs & Centers
- Tufts University-Tufts Medicine Research Enterprise
-
Local & Global Engagement
- Pathway & Enrichment Programs
- Global Health Programs
- Community Engagement
MD Curriculum
Tufts School of Medicine is committed to curricular innovation and improvement as we continually strive towards the next level of educational excellence. Rapid changes in health care delivery, biomedical knowledge and technology require medical students to confront a wide range of new information, practices and issues as they progress through their education. To meet these challenges, more than 200 faculty, students and staff worked to redesign the Tufts’ curriculum to continue to position Tufts’ graduates for success, no matter what field of medicine they choose to pursue. The current curriculum was rolled out in August of 2019 with the class of 2023.
Curriculum Details
-
Tufts is committed to curricular innovation and improvement, and we continually strive towards the next level of educational excellence. Rapid changes in health care delivery, biomedical knowledge and technology require medical students to confront a wide range of new information, practices, and issues as they progress through their education. To meet these challenges, more than 200 faculty, students and staff worked to redesign the Tufts’ curriculum to continue to position Tufts’ graduates for success, no matter what field of medicine they choose to pursue. The new curriculum rolled out in August of 2019 with the class of 2023.
The overall goal of the Tufts curriculum is to graduate compassionate and highly skilled physicians who possess the knowledge, ability, and attitudes to promote the health of individuals and populations. Our students will develop advanced skills in clinical reasoning and communication, allowing them to improve the patient experience while delivering the highest quality care. We will also help students to cultivate skills in personal reflection, mindfulness, resilience, inquiry, and lifelong learning. These tools will ready them to skillfully navigate diagnostic and therapeutic uncertainty and successfully adapt to a constantly changing healthcare environment. Our students will understand the importance of patient-centered outcomes and the processes of patient care at a systems level, including the functioning of interprofessional teams. Tufts’ graduates will be positioned to provide outstanding care by applying a detailed understanding of: the scientific basis of health and disease, healthcare delivery systems (and how to navigate those systems), social determinants of health, and population health (the ability to address the needs of patients and communities).
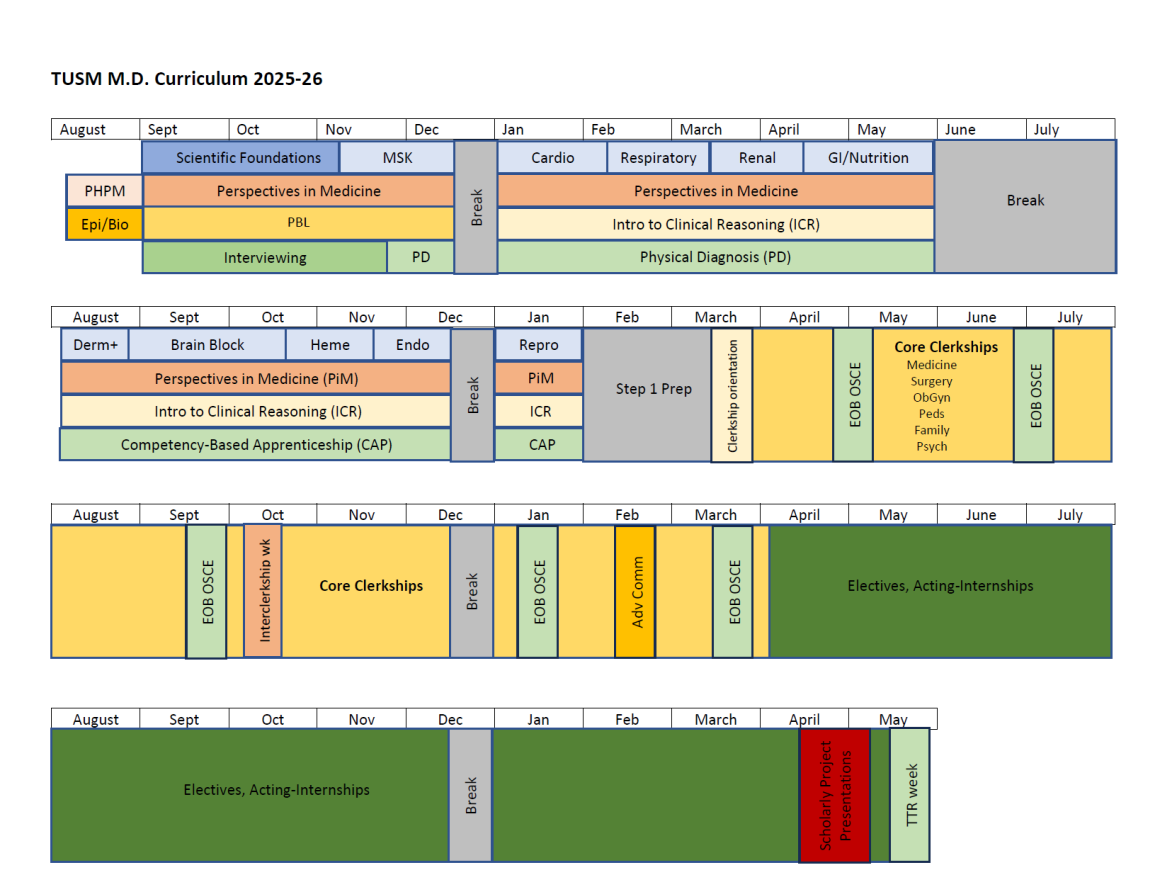
The schematic below shows the organization of the Tufts curriculum which centers on the four-year integration of basic science, clinical science/medicine, healthcare delivery science, and personal and professional development. Four “perspectives” have been developed and designed to be woven throughout the four-year curriculum.
- Healthcare Systems: healthcare costs, healthcare delivery systems, quality and safety, quality improvement, interprofessional collaboration, advocacy, law and reporting obligations, clinical informatics, chronic illness care, team-based care
- Population Health: structural health determinants, health disparities and inequities, public health, prevention, culturally competent care, care of the underserved, active citizenship, global health, social and health justice
- The Patient Experience: advanced communication, shared decision making, impact of health on patient and family life, end-of-life care/palliative care, assessment and management of pain and of substance use disorders
- Personal and Professional Development: wellness, resilience, professionalism, ethical practice, evidence-based medicine, self-regulated lifelong learning, inquiry/discovery, navigating uncertainty, professional identity formation, leadership, teaching, clinical skills, clinical reasoning, advocacy skills.
The pre-clerkship phase of the Tufts’ curriculum (August of year one to January of year two) uses interactive lectures and other forms of active learning (flipped classrooms, small groups, team-based learning) to fully engage students in the educational process. There is a focus on case-based problem solving. Early clinical work allows students to apply classroom learning at the beside. A state-of-the-art clinical simulation and standardized patient program provides abundant opportunity for our students to further refine their clinical skills.
The curriculum commences with an introduction to the healthcare system and the profession of medicine, providing essential context on which to scaffold all subsequent learning. A foundational medical science unit follows, integrating core principles of biochemistry, cell biology, genetics, molecular biology, pharmacology, immunology, microbiology, and infectious disease. Clinically focused organ system units begin in November of year one and run until January of year two. These units integrate anatomy, histology, physiology, pharmacology/therapeutics, pathology, pathophysiology, clinical skills, imaging, and the perspectives (see above). This strong foundation in the pathophysiologic basis of disease is critical to the formation of the expert clinician.
Early in year one students begin two 15-month long sequences. The first, Foundations of Patient Care, builds skills in medical interviewing and physical diagnosis, and culminates in the Competency-based Apprenticeship in Primary Care (CAP). CAP begins in year two with students spending one day a week in a primary care office, working through a core set of competencies focusing on fundamental clinical and communication skills. Afternoon Selectives during year one afford students the opportunity for early career exploration. The second, Foundations of Evidence-Based Medicine and Clinical Reasoning, begins with Problem-Based Learning (PBL), a case-based small group experience designed to develop student’s ability to effectively engage in self-directed learning. The Introduction to Clinical Reasoning Course follows with expert clinicians facilitating small groups to build students’ non-analytic and analytic reasoning skills, refining their ability to diagnose disease while recognizing pitfalls in the diagnostic process.
Core clerkships start during March of year two and consist of eight weeks each of medicine and surgery, and six weeks each of family medicine, obstetrics-gynecology, pediatrics, and psychiatry. An additional eight weeks of electives allow for career exploration, and based on the student’s interest, more advanced work in a variety of disciplines. A one-week intersession period has been created to return students to campus to allow for ongoing integration of the perspectives and advanced skill development. The clerkships allow students to develop clinical skills and to learn to take responsibility for patient care at a number of Tufts affiliate sites representing a wide variety of clinical settings.
During the last block of year three and continuing through year four, students take advanced clinical rotations, including acting internships, a clinical neuroscience rotation, and a wide variety of electives. These experiences expand clinical knowledge and strengthen clinical skills and reasoning, positioning students for success in their first year of postgraduate training. An end-of-year, one-week bootcamp, including extensive simulation experience, provides final preparation for internship.
A spirit of inquiry and commitment to scholarship is an essential component of the Tufts curriculum. Beginning with the class of 2024, all students will complete a scholarly project during the four-year curriculum. The project allows students to pursue an area of interest in detail by formulating a scholarly question, using appropriate methodology to address that question and presenting findings in a scholarly forum. In addition to more traditional basic science and clinical research projects, students’ scholarly work can focus on public health, civic engagement or clinical quality improvement. Two periods of time, one at the end of year three (between the end of the core clerkships and the start of advanced clinical rotations) and another during the middle portion of year four, are reserved for completing the scholarly project.
An important addition to the curriculum will be the implementation of a faculty coaching model designed to ensure that a faculty member has a four-year longitudinal picture of a student’s development of clinical skills and professional attributes. The coach will be the main faculty member responsible for the student’s professional identity development (including resilience, ethical practice, self-regulated lifelong learning, navigating uncertainty), and will also assist in teaching clinical skills, in facilitating self-reflection (meta-cognition) and helping students remediate areas of weakness. The coach will:
- Meet regularly with student
- Review all formative and summative assessments
- Directly observe clinical skills
- Monitor progress toward achievement of competencies.
This model will help to strengthen student connections to faculty members and improve students’ acquisition of skills required to practice medicine in the 21st century. In addition, the coach will be key in identifying students who, though not failing, may need more support/remediation to achieve competency.
-
-
Curricular Themes
Our curriculum emphasizes themes that span all years of a student's education. These are designed to help students understand their future roles as physicians.
The key elements of each of these themes is described below.
Healthcare Systems: healthcare costs, healthcare delivery systems, quality and safety, quality improvement, interprofessional collaboration, advocacy, law and reporting obligations, clinical informatics, chronic illness care, team-based care
Population Health: structural health determinants, health disparities and inequities, public health, prevention, culturally competent care, care of the underserved, active citizenship, global health, social and health justice
The Patient Experience: advanced communication, shared decision making, impact of health on patient and family life, end-of-life care/palliative care, assessment and management of pain and of substance use disorders
Personal and Professional Development: wellness, resilience, professionalism, ethical practice, evidence-based medicine, self-regulated lifelong learning, inquiry/discovery, navigating uncertainty, professional identity formation, leadership, teaching, clinical skills, clinical reasoning, advocacy skills
Description of Required Courses and Core Clerkships
Preclerkship Units/Courses (see schematic)
Population Health and Profession of Medicine (First year, 3 weeks)
This course introduces medical students to fundamental concepts in the areas of public and population health, epidemiology and biostatistics, health care systems, ethics and professionalism. The unit provides an overview of the organization of the US health care system, health inequities, cross-cultural medicine, shared-decision making, quality improvement, preventive medicine, and health care economics. Students actively engage in learning, exploring neighborhoods in the Boston area and applying data from these communities to better understand how physicians can positively impact the health of patients and populations. During interactive team-based learning utilizing clinical cases students apply what they have learned to realistic patient scenarios. The course is based on four content themes in Perspectives in Medicine - Patients, Populations, and Systems, woven throughout the four-year curriculum (see below). This course is integrated with the Epidemiology and Biostatistics Course (see below).
Teaching format: Interactive lectures, flipped classrooms, small group case-based sessions, large group discussions, community field experiences, team-based group exercises, group projects
Scientific Foundations of Medicine Unit (SFM) (First year, 11 weeks)
The SFM unit consists of two courses delivered synchronously: Molecules to Tissues (MTT) and Microbes, Infectious Disease and the Immune System (MIDIS). The unit is further divided into four, three-week sections, each with a unifying theme and concluding with an illustrative patient presentation.
Teaching format: Interactive lectures, flipped classrooms, small group case-based sessions, large group problem solving sessions, team-based learning, patient presentations, and microbiology laboratories.
Molecules to Tissues (MTT)
Molecules to Tissues integrates material essential to the understanding of the scientific foundation of medicine including biochemistry, cell biology, and medical genetics. Core concepts in pathology, pharmacology and histology are introduced.
Biochemistry sessions are designed to provide an understanding of the biochemical basis of physiological processes. While the emphasis is on functional and regulatory aspects of biochemistry that inform understanding of health and disease, a solid knowledge of the structure of major biological substances and of enzymatic reactions is also required to understand physiological function. Biochemistry covers topics in genetic material, molecular cloning and diagnosis, protein and enzyme structure and function, carbohydrate metabolism, lipid metabolism, protein metabolism, nucleic acid metabolism, and cellular energy, with integrative sessions in cancer, diabetes, and starvation. Disease states are used to show how specific biochemical defects can lead to illness. Diseases are highlighted in patient forums (mitochondrial disease, phenylketonuria, lipid catabolism, carnitine transport) and in small groups (chronic myelogenous leukemia, glycogen storage disease, hypercholesteremia, and urea cycle disorders).
Cell biology sessions focus on the relationship between cellular and subcellular structures and mechanisms related to human health and the pathological basis for diseases. Several dozen diseases and human health conditions are discussed in terms of the underlying cellular pathobiology involved, preparing students for the organ-based systems. Students are regularly exposed to research principles and methods that underpin the concepts taught. The social and ethical issues involved in the application of research and treatment advances are highlighted throughout the course. These sessions cover complex cell functions such as cell proliferation and apoptosis, along with cell-cell and cell-matrix interactions. There is discussion of stem cells and the ethical implications of their use.
Medical genetics sessions introduce the basic principles of human genetics and their application to clinical medicine. Topics include genetic patterns of inheritance, DNA diagnostic methods, chromosome abnormalities, dysmorphology, anomalies, teratogens, multifactorial inheritance, cancer genetics, prenatal genetics, arrays, and next-generation sequencing. One of the important skills taught is the translation of a verbal family history into a pedigree diagram that can be used to determine the most likely mode of inheritance of a genetic disorder. Students are guided through calculating the risk of a genetic disorder in a family by working through problems in class. The course provides the framework for students to recognize who might benefit from genetic counseling and the indications for a referral to a geneticist.
Histology sessions are designed to stress the relationships between structural composition and function and relate microscopic anatomy to other biomedical disciplines. In MTT, there is emphasis on epithelium, glands, lymphoid tissues, blood and connective tissue. Important correlations relevant to clinical medicine are emphasized. Information is mainly derived from light and electron microscopy, histochemistry, cell and molecular biology, and biological chemistry. Histology is also integrated into all subsequent organ-based courses.
Core pathology sessions emphasize the cellular and tissue alterations caused by pathologic stimuli. There is a focus on cell injury, cellular adaptation and death, acute and chronic inflammation, neoplasia, atherosclerosis, and circulatory diseases. These sessions set the stage for students to learn organ-specific pathology in subsequent courses.
Core pharmacology sessions introduce basic principles including the pharmacokinetics and pharmacodynamics of medications and their use in clinical medicine. Additional material covered includes sources of drug information, drug development, and pharmacogenomics. This course builds a conceptual foundation for further learning of more disease-specific pharmacology, which is taught in an integrative manner in MIDIS and in the organ-based system courses that follow.
Microbes, Infectious Disease and the Immune System (MIDIS)
Microbiology, Infectious Disease and the Immune System (MIDIS) integrates microbiology, infectious disease, immunology and antimicrobial pharmacology.
Immunology sessions introduce students to the most important principles governing the functions of the human immune system and how these relate to human disease. The principal goal is to demonstrate the relevance of immunology to normal function and its relationship to human disease. Content areas include:
- innate immunity
- the complement system
- B-cell function, formation
- role and function of antibodies
- role of the thymus
- development of T-cells
- cell-mediated immunity
- the major histocompatibility system
- transplantation immunology
- the immunologic basis of tumor immunology
- clinically applied immunology including the immunologic basis of auto-immune disease and the hypersensitivity disorders
- acute and chronic inflammation as a bridge to further studies in pathology congenital and acquired immune deficiency states including HIV infection and ageing
Microbiology sessions increase student understanding of the basic biology of bacteria and viruses as causative agents of human disease. The first section covers bacterial structure and growth, with emphasis on how these processes provide therapeutic targets, as well as control of gene expression. Emphasis is placed on adaptation to growth and survival in the human host and on virulence gene regulation. Bacteriophage biology, both lytic and lysogenic, is described in the context of the expression and horizontal transfer of phage-encoded virulence factors. The role of phage- and transposon-mediated genetic exchange, including antibiotic resistance determinants and virulence factors, in the generation of highly pathogenic bacteria (i.e. “superbugs”), is presented with some mechanistic description.
The virology section describes the interaction of human viruses with mammalian cells. The life cycles of two viruses with different RNA genomes and two viruses with different DNA genomes are used as paradigms for entry, uncoating, viral gene expression, assembly and egress. The role of viruses in human oncogenesis is covered. Finally, the above topics are revisited and synthesized by describing the use of microbes in modern medicine. The utilization of recombinant DNA technology is discussed including the production of recombinant proteins of medical significance and more recent efforts to utilize engineered viruses in human gene therapy.
The Infectious Disease sessions present the basic pathobiology of organisms and the human syndromes they cause. Highlights of physical signs and symptoms, diagnostic strategies and an overview of treatment of infectious syndromes are covered. Specific learning objectives include: identification of specific infectious disease syndromes and their clinical presentation, identification of the mechanisms by which specific microbial pathogens cause major infectious syndromes, and the mechanism of action, spectrum of activity and major adverse reactions of antimicrobials used to treat infections.
These sessions cover mechanisms of pathogen-induced host damage and specific microbial pathogens with an emphasis on identification, encounter, entry, spread/multiplication, virulence factors, damage and clinical manifestations, diagnosis and treatment/prevention. One section covers bacterial pathogens, the syndromes they cause, and the antimicrobials used to treat the pathogens. For example, Staphylococcus aureus is discussed in terms of its key physical features, unique properties, virulence determinants and basis for multi-drug resistance in case-based format that is then highlighted in discussions of infectious disease syndromes that are often caused by the organism such as bacteremia, osteomyelitis, endocarditis and skin and soft tissue infections. Adjoining these sessions, there is discussion of the common antibiotics that are used to treat S. aureus and other organisms causing the syndromes discussed. The second section covers viral pathogens, parasites, mycobacteria and fungi with some emphasis on immunocompromised hosts. While the course does not cover every pathogen, students learn the important relationship of host, pathogen and environment as the basis upon which to understand the pathophysiology of microbial pathogens, the infections they cause and the approach to diagnosis and treatment.
Organ Systems
The organ systems integrate organ-specific cadaveric and virtual anatomy, histology, physiology, pathology, pathophysiology, infectious disease, imaging, clinical laboratory, pharmacology, therapeutics, ethics and the Perspectives in Medicine - Patients, Populations, and Systems. Each unit begins with a focus on normal structure and function and then moves to the pathophysiologic basis of disease. There is emphasis on disease preventions, diagnosis and treatment. Considerable time is devoted to case-based sessions and the approach to patients with most commonly encountered symptoms, signs and laboratory/imaging abnormalities. The Perspectives in Medicine - Patients, Populations, and Systems topics are integrated throughout the organ systems with emphasis on population and public health, social determinants of health, health care disparities, variations in practice, value-based care, health care justice, quality and safety, palliative and end-of-life care, shared-decision making, management of pain and substance use disorder, ethics and professionalism. Wellness is also integrated throughout these units.
Teaching format: Interactive lectures, flipped classrooms, problem solving sessions, clinicopathological conferences, small group case-based sessions, team-based learning, patient presentations, laboratories.
First Year
Musculoskeletal
Cardiovascular
Respiratory
Renal
Gastrointestinal/Nutrition
Second Year
Dermatology
The Brain (Neuroscience, Introduction to Clinical Psychiatry, Addiction Medicine)
Hematology
Endocrine
Reproductive
Musculoskeletal (First Year, 7 weeks)
The Musculoskeletal course covers the physiology, histology, anatomy, pathology and pathophysiology of muscle, nerve, cartilage, bone, joints and synovium. The course introduces the student to cadaveric anatomy with sections on the lower extremity, back and upper extremity. Areas covered in Musculoskeletal include skeletal homeostasis, disorders of bone metabolism, orthopedics, orthopedic emergencies, osteoarthritis, rheumatoid arthritis, Lyme spondyloarthropathy, fibromyalgia, crystal induced joint disease, bone and joint infections, bone and soft tissue tumors, systemic lupus erythematosus, scleroderma, pediatric orthopedics and rheumatology, vasculitis, and radiology of the musculoskeletal system. Pharmacology sessions focus on antirheumatic agents, non-steroidal anti-inflammatory drugs, opioids, and local anesthetics.
Cardiovascular (First Year, 5 weeks)
This unit takes an integrated approach to the diseases of the cardiovascular system. The goal is for students to develop the analytical and cognitive skills necessary for a successful transition from basic cardiovascular physiology to the care of the patients with cardiovascular disease. The unit provides an introduction to normal and abnormal hemodynamics directed at three major areas; shock, heart failure and valvular heart diseases. The contemporary use of hemodynamic data to help diagnose various pathophysiological states is highlighted. The course covers the epidemiology, risk factors, clinical manifestations, and management (including anti-ischemic therapy) of coronary artery disease. There is a broad review of the different types of dyslipidemias, and the pharmacological agents used to treat lipid disorders. Subsequent sessions cover the etiology, clinical manifestations, natural history and management of heart failure, valvular heart disease, and peripheral vascular disease (including cerebrovascular diseases, aortic dissection, aortic aneurysms, diseases of the vascular supply to the lower extremities and venous diseases). Sessions are dedicated to the basics of electrocardiography and the identification of arrhythmias. Students learn the cellular pathophysiology of the latter along with clinical manifestations and pharmacologic management.
Respiratory (First Year, 5 weeks)
The overall objectives of this course are to provide the student with a strong foundation of basic respiratory physiology, histology, anatomy, pathophysiology, pharmacology, and pathology that will serve as a foundation for future learning. The course covers the pathophysiology, clinical and pathologic manifestations, diagnostic evaluation and therapeutic approach to a broad spectrum of respiratory disease categories including obstructive (airways), restrictive (including parenchymal), occupational and environmental, infectious, vascular, neuromuscular, pleural, and neoplastic. This unit also covers diseases of the upper airways. Dissection of the thorax and the neck is used during the respiratory course, while also preparing students for the subsequent cardiovascular course. Considerable time is spent learning how to interpret the major diagnostic modalities used in respiratory medicine including pulmonary function tests, chest radiology (chest x-rays and chest CT scans) and arterial blood gases. There is a strong emphasis on clinical correlation, allowing students to link abnormal symptoms and signs with the underlying pathophysiologic processes.
Renal (First Year, 4 weeks)
The kidneys play a central role in the maintenance of the internal milieu by balancing fluid, electrolytes, and hydrogen ions to provide optimal conditions for molecular, cellular, and body system functions. They also serve as the major excretory organ for metabolic byproducts, drugs, and other organic substances. Finally, the kidneys are an important endocrine organ, producing vasoactive factors, erythropoietin, and other circulating hormones. As such, the kidneys are intricately involved in volume regulation and systemic hemodynamics. The importance of the kidneys is most clearly demonstrated in the presence of disease states. The Renal Course explores disorders that arise from primary defects in kidney function, as well as how the kidneys respond to extra-renal disturbances. Pathologic injuries to the architecture and structure of the nephron and kidneys, and the impact of immunologic, genetic, toxic, and idiopathic processes are discussed. Finally, the Renal Course explores the pathogenesis and therapy of chronic kidney disease, and the consequences of kidney failure. Anatomic dissection of the kidneys, ureter and bladder allows for structure function correlation.
Gastrointestinal (First Year, 7 weeks)
The Gastrointestinal course (oral cavity, esophagus, stomach, small intestine, colon, liver, gallbladder, and pancreas) covers the physiology, histology, anatomy, pathology, pathophysiology, and the pharmacologic approach to treatment of diseases of the gastrointestinal system. A case-based approach is used both during interactive lectures and small group sessions. Many sessions are co-taught by a clinical gastroenterologist and gastrointestinal pathologist using a clinicopathologic conference approach where the pathophysiology is presented first followed by the pathology of the particular disorder. Common disorders of luminal gastrointestinal disease and diseases of the liver, pancreas, and gallbladder are reviewed including allergic, medication-induced, autoimmune, inflammatory, infectious, and neoplastic disorders. The Gastrointestinal course is tightly integrated with the synchronously taught Nutrition course.
Nutrition (First Year, 7 weeks)
For decades, Tufts has taught a full course in nutrition in the first year and reinforced these themes in the clerkship year. Diet has a profound impact on maintenance of health and development of disease. In turn, acute and chronic disease substantially influence nutrient needs and the ability of patients to consume, digest, and assimilate nutrients. The foundational nutrition course addresses the fundamental relationships between diet, nutrients, health, and disease. The primary focus is on nutritional issues encountered by the practicing clinician. Basic science concepts, including topics from biochemistry, physiology, pathophysiology, and medical specialties, are incorporated. Students receive instruction in assessment of nutrition status in the outpatient and inpatient settings, nutritional support, guidance on nutrition counseling, and the roles of other health professionals including dietitians and speech-language and swallow therapists. Topics include nutritional content of foods; macro- and micronutrients; obesity; malnutrition; selected micronutrient deficiencies or excess; nutrition across the lifespan including children, pregnant patients, and the elderly; eating disorders; allergies and intolerances; food security; popular diets; and dietary supplements. In the clerkship years, students practice interpreting nutrition labels; counseling patients on nutrition accounting for age, medical conditions, and social determinants; using motivational interviewing for behavioral change as related to diet; assessing patients’ nutritional status via history, clinical measurements, and labs; and working with other health care professionals to optimize patients’ nutrition and health.
Dermatology (Second Year, 2 weeks)
The Dermatology course is designed to introduce students to the specialty of dermatology through emphasis on the proper description of entities and the development of differential diagnosis, the pathogenesis of common dermatologic diseases and the treatment of many of these dermatologic entities. The course includes elements of physical diagnosis including understanding of the dermatologic lexicon, bedside diagnostic testing and the pathogenic mechanisms of skin disease. In addition, there is a focus on such entities as acne, psoriasis and other papulosquamous disease, eczematous dermatitis, skin cancer and the dermatologic mechanisms of skin disease. Discussion of these entities includes pathogenesis, diagnosis and treatment with a focus on appropriate pharmacology as well. Infectious disease topics include: approach to the febrile patient, approach to the immunocompromised host, zoonotic diseases, vector-borne illness, and sexually transmitted disease. There is also a review of major infectious disease syndromes and an antibiotic refresher.
The Brain (Second year)
Neuroscience (Second Year, 6 weeks)
The Neuroscience course presents an orderly view of neuroanatomy starting with the spinal cord and ascending up the neuroaxis to the brainstem, cerebellum, basal ganglia diencephalon and cerebral cortex. The presentation of the anatomy of each major nervous system region is followed by sessions relating the anatomy to localization of lesions and disease in that region of the central nervous system. A final segment of the course covers clinical and pathologic features of neurologic diseases such as Parkinson’s Disease, Huntington’s Disease, dementias, multiple sclerosis, epilepsy, stroke, brain tumors, head trauma, disturbances of consciousness, malformations, and infections of the central nervous system. A major emphasis is on developing a clinical approach to patients with common neurologic symptoms and signs. The teaching faculty includes neuroscientists, neurologists, neurosurgeons, and neuropathologists.
Clinical-anatomic correlations are reinforced throughout the course in problem-solving small-group sessions in which students meet with neurologists. Students are asked to localize lesions and to predict the etiology based on case histories of patients with neurologic diseases. In addition, there are anatomy laboratories for the course that are based on computer programs developed by the course directors and prosections in the anatomy laboratory. These laboratory exercises are designed to further reinforce clinical-anatomic correlations. Students also learn the physical examination of the neurologic system (including ophthalmology).
Principles of Addiction Medicine (Second Year, 3 weeks)
The Principles of Addiction Medicine course addresses the mechanism of action of major classes of drugs of abuse (alcohol, opioids, psychostimulants, cannabinoids), their acute and chronic effects on central neurotransmitter systems and pathways, and their receptor targets. The course further introduces the foundations of the clinical practice of Addiction Medicine, from differential diagnosis of drug-associated toxidromes to tools for patient interviewing, screening and evaluation, levels of clinical care of addiction, group addiction recovery programs, and methods and approaches to address prescription drug abuse.
The course includes sessions with patients who have successfully addressed their addiction, with physicians who play a prominent role in 12-step and cognitive/behavioral intervention addiction recovery programs, and with the directors of the Physician Health Services of the Massachusetts Medical Society who discuss the special challenges facing the chemically-dependent physician. These sessions also introduce gender and diversity issues in addiction and addiction recovery. The students actively integrate the material by attending at least one addiction recovery meeting either through the AA or a cognitive and behavioral intervention program, as observers in small groups and record and discuss their experience.
Introduction to Clinical Psychiatry (Second Year, 3 weeks)
Introduction to Clinical Psychiatry focuses on known neurobiological aspects of psychopathology and its treatment. Though it introduces medical students to the diagnosis of major psychiatric conditions, it also demonstrates the phenomenology of the conditions. Major conditions that are discussed include depression, bipolar disorder, anxiety disorder, schizophrenia, somatoform disorders, personality disorders, childhood disorders, cognitive disorders, and eating disorders. Each of these sessions is closely integrated with sessions on psychopharmacology. In this manner, students learn to diagnose and, then, treat the conditions in an organized and coherent manner. A major emphasis is on developing a clinical approach to patients with common symptoms and signs of psychiatric illness. The course also emphasizes the developmental perspectives that contribute to psychopathology including sessions on the development of personality and character, and theories of psychological development.
Hematology (Second Year, 5 weeks)
The Hematology course is divided into 3 major areas: (1) the normal physiology of the blood, including cellular and fluid phase components, (2) the major malignant diseases arising from blood and bone marrow, and (3) a conceptual framework for understanding the epidemiology, evaluation, and management of the non-hematologic malignancies (the “solid” tumors). The course also integrates pharmacology pertaining to hematology and oncology, basic concepts in pathologic diagnosis of malignancies, and blood bank and transfusion medicine. Specific topics that are covered include the physiology of the bone marrow, hematopoiesis, and coagulation, along with non-malignant diseases arising from absence or dysfunction of blood elements, transfusion medicine (including blood groups, transfusion components, and transfusion reactions), acute and chronic leukemias, Hodgkin’s and non-Hodgkin’s lymphomas, plasma cell disorders, myeloproliferative neoplasms, myelodysplastic syndromes, hematopoietic stem cell transplant, epidemiology of solid tumors, and the pharmacology of anti-coagulants, pro-coagulants, and anti-neoplastic agents. The course is integrated with the other organ-system courses, most of which provide additional coverage of malignancy.
Endocrine (Second Year, 4 weeks)
The Endocrine course is designed to give an integrated overview of the endocrine systems of the body from the perspective of normal physiology and disease states. The course starts with an introductory session including general concepts of endocrine physiology, pathology and pathophysiology. Following this, the course is divided up into subsections based on a specific endocrine gland including adrenal, thyroid, parathyroid/calcium, endocrine pancreas and pituitary. Each of these subsections starts out with a discussion of the normal physiology of the system followed by discussions of major disease processes including hyperfunction, hypofunction and neoplasia with a clinical approach to diagnosis and treatment and relevant concepts in pathology. The Endocrine unit covers hypothyroidism, hyperthyroidism, autoimmune thyroid disease, thyroid nodules, diabetes mellitus, hypoglycemia,diabetes insipidus, pituitary insufficiency, Cushing’s disease, Addison’s disease, hypocalcemia, hypercalcemia, hyper- and hypoparathyroidism, osteoporosis, obesity and endocrine neoplasms.
Reproductive (Second Year, 4 weeks)
The Reproductive course starts with normal development of the reproductive tract and then moves to structural abnormalities such as Mullerian defects and genetic deficiencies causing disorders of sexual differentiation. The hypothalamic-pituitary-gonadal axis is discussed including disorders to this system leading to oligospermia, testosterone deficiency, anovulation and menstrual irregularity. Issues important in the menopause including menopausal symptoms, pelvic organ prolapse and urinary incontinence are covered. Normal and abnormal pubertal development is reviewed. There is comprehensive discussion about contraception methods. Management of unintended pregnancies is also reviewed. Normal and abnormal pregnancy is introduced with lectures focusing on preconception health, prenatal care, labor, birth and disorders that can develop including pregnancy-induced hypertension and antepartum bleeding. Maternal pathophysiology, first trimester bleeding, miscarriage, ectopic pregnancy, disorders of the postpartum period, breastfeeding and the effects of drugs in pregnancy and lactation are subsequently discussed. Causes of pelvic pain, genital infections and infertility are also reviewed. Female sexual response as well as sexual dysfunction and abuse are covered. Pathology of the breast, cervix, ovary, and uterus are taught along with the evaluation and treatment for disorders in these organs including uterine fibroids, polyps, hyperplasia, cancer and cervical dysplasia and cancers. The male reproductive tract is covered starting with gametogenesis, normal physiology of erection and ejaculation, disorders of male sexual function including impotence and infertility. Pathology of the male genital tract covers prostatic hyperplasia, cancer, priapism, and testicular torsion. Additional topics in issues in LGBTQ health and transgender medicine.
Foundations of Patient Care
Medical Interviewing and the Doctor-Patient Relationship (MIDPR) (First year, 12 weeks)
MIDPR, starting in August of first year, is designed to introduce students to the art and science of the medical interview. The goals of the course include: providing an introductory experience in talking to patients, learning about the doctor-patient relationship, learning basic interviewing and history taking techniques, learning about the patient’s experience of illness, introducing the write-up and presentation of the clinical experience, increasing awareness of and ability to talk about topics that are difficult (nutrition, sex, drugs, spirituality, death), and learning to talk with children, the elderly, and the dying. Sessions on human development are integrated into the unit.
The specific competencies that the course aims to develop includes: professionalism, rapport, empathy, medical history, patient-centered perspective, growth towards physician role, oral presentations, written documentation, group participation, constructive feedback, and reflective practice. The course is offered on Wednesdays from the end of August through the middle of November and consists of morning presentations/demonstration interviews followed by afternoon small group sessions where, under the supervision of a section leader, students interview patients in hospitals and at elderly housing sites. Students spend two sessions at an elderly housing site, six sessions at a hospital (Tufts Medical Center, Lahey Hospital and Medical Center, St. Elizabeth’s Medical Center, Newton-Wellesley Hospital, or South Shore Hospital), and two sessions in the Clinical Skills and Simulation Center (see below).
The course also includes a practical experience of interviewing with an interpreter as well as two practical experiences interviewing simulated patients in the Clinical Skills and Simulation Center (CSSC). An Objective Structured Clinical Examination (OSCE) serves as a final examination with all students having to demonstrate competence in the course’s learning objectives before progressing to the next part of the Foundations of Patient Care.
Teaching format: Interactive sessions, patient presentations and demonstration interviews, small groups in clinical settings, standardized (simulated) patient interviews in the CSSC.
Physical Diagnosis (First Year, November to May)
The Physical Diagnosis Course teaches the clinical skills of the basic, normal physical examination, as well as serving as an introduction to the abnormal physical examination. The course is tightly integrated with the organ-system units. Students systematically learn the physical examination of the following regions: lower extremity, back and spine, upper extremity, cardiovascular, respiratory, abdominal, genito-urinary, mental status, otorhinolaryngologic, ophthalmologic and neurologic. Lectures emphasize basic techniques and clinical correlations. Evening sessions in the Clinical Skills and Simulation Center begin with a demonstration following by practice under faculty supervision. Simulation task trainers (manikins) are used to learn normal and abnormal findings. Students further refine their skills through practice sessions with standardized patients. Ultrasound is incorporated into many of the sessions.
Teaching format: interactive lectures, case presentations, physical exam demonstrations, small groups in the CSSC, standardized patient practice sessions, and ultrasound.
Competency-based Apprenticeship in Primary Care (CAP) (Second Year, 18 weeks)
The CAP course builds on the foundation established in the interviewing and physical diagnosis courses. Working in pairs, students spend one full day a week in an outpatient clinic or office in Family Medicine, General Internal Medicine or Pediatrics. CAP starts during the last unit of first year and continues through early January of second year. Students refine their clinical skills in taking an accurate medical history and performing both complete and focused physical examinations. Students learn how to structure a differential diagnosis, counsel patients, document the medical encounter (usually with an electronic medical record), organize and deliver concise oral presentations, and how to perform basic office procedures. Concepts learned in the organ-system units are applied in the clinical setting.
The ambulatory experience is supplemented by interactive workshops including introduction to office setting, documentation and presentation, basic office procedures, lifestyle modification counseling, physical diagnosis review, breast and pelvic examination, caring for children and adolescents, and advanced communication.
Teaching format: clinical work in primary care setting, interactive workshops, standardized patient sessions, self-directed learning
Foundations of Evidence-based Medicine and Clinical Reasoning
Epidemiology and Biostatistics (First Year, 3 weeks)
The primary goal of the course is to teach students the skills to read, understand and critique the medical literature. This course covers descriptive epidemiology, randomized controlled trials, cohort studies, case control studies, external and internal validity, bias and confounding, screening, sources of bias in epidemiologic studies, and a series of sessions on biostatistics. Extensive use is made of the small group setting to reinforce and apply concepts. Considerable time during small group is used to analyze key examples from the medical literature. Using a target article, students write a paper critique where they discuss: sources of bias, the effect each source of bias had on the study results, whether the authors fairly acknowledged limitations of the study, the internal and external validity of the study, the evidence for/against causal associations and, a statement regarding the attributable risk and the related public health significance of such data. The course lays the foundation for the Introduction to Clinical Reasoning Course.
Teaching format: small groups
Problem-Based Learning (PBL) (First Year, 18 weeks)
The PBL course uses a small group learning venue to introduce students to medical evidence and clinical reasoning. Virtual patient cases are explored that contain embedded elements inspired by the basic science principles contained within the curriculum. Students work collaboratively to discuss, explore, and understand clinical issues present in common health care problems that illustrate and integrate these basic science principles. In this environment of active learning students demonstrate the ability to acquire new knowledge, apply new skills, and convey new attitudes required of a medical professional.
The members of each small group meet together for two-hours each week and remain together over the course of one semester. Each group consist of five students and two faculty facilitators who alternate weeks (one of the facilitators is the students’ faculty coach). The principal learning goals are: (1) students will demonstrate the ability to direct their own learning independently and their group learning collaboratively as members of a team; (2) students will demonstrate the ability to actively engage in analysis and discussion of health care problems with a group of peers; (3) students will demonstrate the ability to research clinical questions effectively utilizing a variety of information resources; (4) students will demonstrate the ability to present information to a group of peers and to teach effectively; and, (5) students will demonstrate the ability to give and to receive constructive feedback with a group of peers and with a facilitator.
Teaching format: small groups case-based discussions, independent research, self-directed learning
Introduction to Clinical Reasoning (ICR) (First and Second Year, January of first year to January of second year)
ICR starts with an introduction to evidence-based medicine designed to build on the information taught in the Epidemiology and Biostatistics and Problem-based Learning courses. This portion of the course is taught using an interactive team-based learning approach. Students are taught the difference between disease-oriented evidence and patient-oriented evidence. Students gain experience in the critical evaluation of research evaluating treatments and diagnostic tests as well as the evaluation of clinical practice guidelines and review articles, including meta-analyses. Students are introduced to Bayes’ theorem and dual process theory, which prepare them for further teaching in clinical reasoning.
The subsequent portion of the course stresses the dual process model of clinical reasoning: non-analytic reasoning (e.g. pattern recognition) and analytic reasoning (e.g. hypothetico-deductive). The course is taught in 15 symptom-based weeks (e.g. chest pain, dyspnea, fever, weakness). To teach non-analytic reasoning, students complete three cases for each symptom. This provides students with an opportunity to recognize the illness scripts of many common diseases and review the differential diagnosis for a given symptom. The course highlights causes of diagnostic error within these cases, teaching students about heuristics. It encourages students to develop metacognition by having them reflect on cases and their diagnostic errors. For the analytic reasoning component, students estimate or calculate pre-test probabilities and apply likelihood ratios to determine post-test probabilities for diagnoses they are considering. There is an emphasis on how clinicians wrestle with diagnostic and therapeutic uncertainty.
Teaching format: team-based learning, small group case-based discussion, online cases, self-directed learning.
Required Core Clerkships
Required core clerkships emphasize the refinement of clinical skills, clinical reasoning, and professional identity formation. A major focus is using the history and physical exam to gather information to generate a prioritized differential diagnosis and an evidence-based diagnostic and therapeutic plan. Students strengthen their skills in interpreting diagnostic test results, documenting the clinical encounter in the electronic health record, delivering an oral presentation of their findings, and transitioning care of their patients to other team members. Each rotation includes an element designed to improve the student’s capacity for interprofessional collaboration. Advanced communications skills are further developed during the clerkships and during intersessions that also integrate content from Perspectives in Medicine -- Patients, Populations, and Systems. Each clerkship in the third year culminates with an OSCE (objective structured clinical exam) or oral exam in addition to the National Board of Medical Examiners Subject Exam (mini-board or "shelf" exam). A strength of Tufts University School of Medicine is its affiliation with various hospitals and other clinical sites across New England, giving students access to rotate with faculty caring for patient populations in urban, rural, and suburban settings across an educationally meaningful variety of communities.
Family Medicine (6 weeks)
The Family Medicine Clerkship is a chiefly outpatient primary care experience that offers an opportunity for students to address a broad array of clinical issues affecting diverse patient populations. Students spend, on average, four days each week in the ambulatory setting working closely with a Family Medicine faculty preceptor. One day per week is spent as a cohort in didactic sessions that feature case-based teamwork and interactive workshops. The workshops include sports medicine, reproductive health, information mastery, nutrition, and navigating the healthcare system.
In the Family Medicine Clerkship, students learn how to approach patients with health concerns across the lifespan in a variety of social contexts. Students develop skills in formulating a differential diagnosis and patient-centered plan for acute concerns, managing chronic conditions, and maintaining individual and community wellbeing with a preventive health approach. There is an emphasis on advanced communication techniques, translating high-quality medical evidence into clinical recommendations, and leveraging longitudinal relationships to support patients' thriving in their communities.
- Clerkship Director: Anita Mathews, MD, MPH
Internal Medicine (8 weeks)
The medicine core clerkship is intended to provide students with a basic understanding of common internal medicine problems. Students see a wide array of illnesses, many of which involve interactions with other medical specialties such as surgery, psychiatry, and interventional radiology/radiology. The mandate of the clerkship is broad and aims to have the student learn common symptoms, signs, and interpretation of laboratory findings; structuring a differential diagnosis and determining the management of common internal medicine problems; effective communication with patients, team members and consultants; ethical issues, documentation, and professionalism. Considerable emphasis is placed on refining clinical reasoning skills.
The clerkship sites range from community hospitals to tertiary care centers in the greater Boston area; Portsmouth, New Hampshire; and Portland, Maine. Despite this diversity, the program ensures that all students are exposed to the same core curriculum and emerge with the same standard set of competencies. The sites offer a variety of lectures and interactive forums and sessions dedicated to direct observation of students by faculty. Regular meetings of the site directors ensure consistency in the experiences and allow the sites to draw upon the experiences of one another. Students are required to document their experiences in an on-line (Canvas) patient log, which allows the site director to make sure that each student has had the requisite exposures by the end of the clerkship.
- Clerkship Director: Laura Snydman, MD, FACP
Obstetrics and Gynecology (6 weeks)
During the Obstetrics and Gynecology clerkship, students engage in a breadth of clinical experiences, ranging from prenatal care and childbirth to preventive gynecologic care throughout the lifespan. Students care for patients amidst some of the most emotional and memorable experiences of their lives, including pursuing infertility treatments, making difficult reproductive choices, facing cancer or infection, and going through childbirth. Students complete their clerkship at one of seven clinical sites, and they are expected to cover a core curriculum of basic gynecologic and obstetric conditions. All sites share common learning objectives, with didactic sessions complementing the clinical education. Simulation-based learning also occurs at TUSM during the rotation. The clerkship consists of both inpatient and outpatient experiences and may include both generalist and specialty services.
- Clerkship Director: Zoe Kiefer, MD, MPH, FACOG
Pediatrics (6 weeks)
The Pediatrics core clerkship incorporates a variety of clinical and teaching experiences to give students experience in the fundamentals of pediatric medicine, as well as exposure to the breadth of pediatrics as a career. The core clerkship consists of outpatient clinical experiences ranging from academic practices to community private practices. Some students participate in inpatient clinical experiences across various local/regional children's hospitals. Students will gain experience in primary care pediatrics and acute care pediatrics, including all ages from newborns through adolescents and young adults. They will learn the nuances required to care for children, adolescents, and their families. The Pediatrics clerkship uses the interactive online Aquifer cases as a standard curriculum across all sites. Many students participate in local clerkship-specific classroom learning or may join pediatric residency learning when at various inpatient-based clinical environments. Pediatric clerkship objectives are adapted from the COMSEP (Council on Medical Student Education in Pediatrics) General Pediatrics Curriculum.
- Clerkship Director: Charles (Chas) Hannum, MD
Psychiatry (6 weeks)
The Psychiatry core clerkship incorporates a variety of clinical and didactic opportunities to give students experience in the fundamentals of psychiatry as well as exposure to the breadth of venues in which psychiatrists practice and contribute to the health care system. The core clerkship consists of inpatient, consultation/liaison, emergency and outpatient sites, working with both adult and child patients suffering from acute and chronic psychiatric conditions. Students learn the fundamentals of the psychiatric history, mental status examination, comprehensive medical record review, and the importance of collateral information in the treatment of psychiatric patients as well as the full range of psychiatric therapeutic modalities (psychopharmacology, verbal psychotherapies, electroconvulsive therapy, etc.). A didactic series of talks introduces students to the basics of the major topics in psychiatry through case presentations that supplement the general experiential curriculum. The competency-based goals and objectives for the psychiatry clerkship were created by the clerkship site directors. Students receive ongoing feedback about their skills particularly around interviewing, forming a differential diagnosis and communication with other members of the health system.
- Clerkship Director: Jody Schindelheim, MD
Surgery (8 weeks)
The Surgery Clerkship provides students with an introduction to a wide spectrum of surgical diseases and their management. Formalized didactics including case studies, case presentations, and Simulation Center experiences that are specifically designed for core clerkship medical students, whereby Surgery faculty teach the presentation, diagnosis, and management of common surgical illnesses. The experiential components of the clerkship include active participation in a wide variety of operative cases, surgical outpatient evaluation and follow-up visits, and as part of an inpatient surgical team. During on-call assignments, students participate in emergency consultations, emergency operations, and trauma activations. The goal of the clerkship is to familiarize students with common surgical pathology and their management and to give students an authentic and broad-based surgical experience.
While there is a diversity of venues, the didactic program ensures that all students are exposed to the same core curriculum and emerge with the same standard set of competencies. In addition to the core case studies, each clerkship site offers a variety of lectures and interactive sessions with faculty, fellows, and residents. Students have access to the Behind the Knife Medical Student Course including supplemental Podcasts. Regular meetings of the site directors ensure consistency in the experiences and allow the sites to draw upon the each other’s' experiences. Students are required to document their clinical experiences in an online patient log, which allows the site director to confirm that each student has had the requisite clinical exposure. Student performance is assessed through standardized multiple choice and oral examinations, a brief oral presentation, and faculty / resident assessment of clinical performance.
- Clerkship Director: Benjamin Johnson, MD
Longitudinal Integrated Clerkship – Maine Track (9 months plus immersion experiences)
Maine Track students may complete a Longitudinal Integrated Clerkship (LIC), spending nine months at one of eight sites. Between two and four students are assigned to each site. Each LIC site has an overall site director and discipline-specific preceptors. Each week (on average) students have one half-day outpatient sessions in family medicine, medicine, obstetrics-gynecology, pediatrics, psychiatry and surgery. In this context, LIC students care for a panel of patients including following these patients, as needed, into the hospital, operating room, labor and delivery, and to consultants. Students have weekly shifts in the emergency department. Inpatient experiences occur as students follow their outpatients who are admitted to the hospital. Students gather monthly at one of the sites for a series of didactic sessions. Based on availability, the LIC is also open to Tufts School of Medicine students who are not in the Maine Track.
Each LIC student additionally completes one or two, four-week immersion blocks consisting of inpatient rotations at Maine Medical Center (or other major Tufts School of Medicine teaching affiliate) and elective rotations. At least one immersion (usually Medicine or Surgery) precedes the LIC portion of the year. The LIC discipline-specific objectives and required clinical encounters are identical to those used in the block core clerkship rotations at Tufts School of Medicine. LIC students are required to complete the same set of virtual online cases and same set of examinations as block core clerkship students.
Neurology (4 weeks)
The neurology clerkship incorporates a breadth of clinical experiences in the inpatient and outpatient settings to give students an understanding of the fundamentals of clinical neurology, including neurological history taking, neurological examination, generation of neurological differential diagnoses, and developing neurological diagnostic and therapeutic options. Considerable emphasis is placed on developing neurological history taking, refining neurological examination technique, and establishing appropriate clinical reasoning skills and neuro-localization principles needed to generate appropriate neurological differential diagnoses.
The neurology clerkship is based in four clinical sites with a standardized core curriculum including learning objectives, standardized patient logs, weekly Monday didactic sessions, and a robust collection of additional educational materials on the intranet (Canvas).
- Clerkship Director: Terrence Li, MD
Perspectives in Medicine - Patients, Populations, and Systems Threads
Perspectives in Medicine (Perspectives) is a longitudinal course that focuses on content outside of basic medical science and the organ systems. The Perspectives - understanding the patient experience of medicine, the organization and effects of our healthcare system, the way population health works, and personal and professional development – are key to becoming a physician.
Perspectives continues the content that is introduced in Population Health and the Practice of Medicine (PHPM), which gives students a foundation in population health, prevention, social justice, and the patient perspective. Perspectives then “sheds light” on many of the same topics through the rest of the curriculum. Perspectives sessions are placed throughout the basic and clinical sciences blocks and are integrated with the beginning of clinical interviewing and patient care.
- Healthcare Systems: healthcare costs, healthcare delivery systems, quality and safety, quality improvement, interprofessional collaboration, advocacy, law and reporting obligations, clinical informatics, chronic illness care, team-based care
- Population Health: structural health determinants, health disparities and inequities, public health, prevention, culturally competent care, care of the underserved, active citizenship, global health, social and health justice
- The Patient Experience: advanced communication, shared decision making, impact of health on patient and family life, end-of-life care/palliative care, assessment and management of pain and of substance use disorders
- Personal and Professional Development: wellness, resilience, professionalism, ethical practice, evidence-based medicine, self-regulated lifelong learning, inquiry/discovery, navigating uncertainty, professional identity formation, leadership, teaching, clinical skills, clinical reasoning, advocacy skills
-
Several programs are also available to students. Participation in Students as Teachers and Community Service Learning is required for graduation. Students may also participate in the Selective program. The Selective program is optional.
Community Service Learning (CSL)
All medical students spend at least 50 hours working directly in the community as collaborators, mentors, and educators. These first-hand experiences enable students to understand health disparities while honing the clinical, communication, and teamwork skills that are essential to their work as physicians. CSL experiences address a range of health issues and patient populations. The Sharewood Project, a free health care organization that is managed primarily by first- and second-year students, is just one example of the ways students can volunteer their time while also developing their clinical skills. Each CSL project provides students with the tools to identify and address the complex factors that influence health inequities.
Learn more about Community Service Learning.
Scholarly Project Program (SPP)
The Scholarly Project (SP) is a mentored project based on each student’s personal passion.
Projects may range from bench or clinical research, to advocacy, to the humanities, to medical education. Students are the primary drivers of projects, working with mentors who provide knowledge, skills, and experience to support students in the design, execution, writing, and presentation of their work. Students may join existing projects or group projects. Credit for the SP is granted based on completion of all requirements (see list below) by the spring of their 4th year. Grading is Credit/No Credit. Program Goals include: fostering curiosity and self-directed learning and developing the scholarly skills necessary to address questions relevant to medicine.
Program Objectives include all students being able to 1. Formulate scholarly questions relevant to the field of medicine; 2. Apply knowledge of study design and data analysis to the appraisal of the healthcare literature and other information; 3. Demonstrate an analytic approach to scientific inquiry including a critical evaluation of the work done; and 4. Present a scholarly product. Students will be assessed on their ability to evaluate a clinical/medical education/health policy/health care delivery question; the ability to gather the data to answer the question (could be literature review); and obtain and present an outcome. SPP modules
MD/MPH students are exempt. Otherwise, all other students are required to fulfill the SPP modules. The students enrolled in the MD/MBA, MD/PhD and research concentration programs will fulfill the scholarly project portion through their programs.
Rebecca Lufler, PhD, Boston Program Co-Director rebecca.lufler@tufts.edu Kate Eastwood, Boston Program Administrator kate.eastwood@tufts.edu Kinna Thakarar, DO MPH, Maine Program Co-Director Kinna.thakarar@mainehealth.org Ilona Wentworth, Maine Program Administrator Ilona.Wentworth@mainehealth.org Selectives (First Year, Tuesday afternoons)
Selectives offer a unique opportunity for students to supplement their core curriculum by sampling a wide range of experiences. Through the Selective Program, students can select from a broad spectrum of various disciplines and practice settings to gain an early introduction to clinical medicine and related areas. Past students have found the Selective Program an invaluable means by which to partner with faculty role models and to identify possible future career paths. There is no standard format for a Selective. The vast majority of Selectives occur in the clinical setting but also may be in the form of seminars, laboratory, selected readings, or a combination. Selectives may involve one student or a group of students. Selectives are offered on Tuesday afternoons, at a variety of sites, both on and off the medical school campus.
-
The goals and objectives, content, and means of assessment in the Maine Track curriculum are the same as those for the traditional track based in Boston. Owning to the Maine Track’s emphasis on the practice of medicine in the state of Maine, there are several differences in how the content is delivered. Maine Track students complete the first year in class with Boston students, moving to Maine for the second year of courses and remaining in Maine for the remainder of the curriculum. The move to Maine for the second year provides students the ability to complete the Competency-based Apprenticeship in Primary Care in a rural setting if desired. After the transition to Maine, the individual courses taught in Maine for the remaining portion of the preclerkship curriculum have identical core learning objectives, content, and assessments as the versions taught in Boston. The smaller number of students in the Maine Track allows for smaller class size for individual sessions. The courses delivered in Maine include Introduction to Clinical Reasoning (begins in Boston with Maine-based faculty), Community-based Apprenticeship in Primary Care, Neuroscience, Addition Medicine, Introduction to Clinical Psychiatry, Reproductive Endocrinology, Hematology, Endocrinology, and Dermatology. For all of these courses taught in Maine, the Boston and Maine co-course directors work closely together to design and deliver the curriculum.
A major difference is in the Core Clerkship year where approximately half the Maine Track students participate in the Longitudinal Integrated Clerkship (LIC). The LIC is run at multiple sites throughout Maine ranging from the 673-bed Maine Medical Center to 25-bed critical access hospitals in rural settings. While in the LIC, students complete the core clerkships under the direction of individual faculty members in each of clerkships. The LIC is augmented by group didactic days and simulation experiences. The LIC is characterized by the development of strong and longitudinal relationships with faculty members who serve as teachers, guides, and mentors. The other half of Maine Track students complete the Core Clerkship year in a more traditional block model that is largely centered at Maine Medical Center. The Advanced Clerkship year is similar to that for Boston students, although Maine Track students are required to complete a number of rotations in Maine.
The emphasis on healthcare in the state of Maine is further enhanced by attention to the Maine or “Dirigo” thread. This focus includes incorporation of topics pertinent to Maine and rural healthcare including health care disparities and health care delivery in rural areas (including a concentration on primary care and prevention), healthcare transformation, inter-professional practice, and the physical and emotional wellbeing of the professionals practicing in rural settings.