-
About
- Departments & Offices
-
Academics
- Public Health
- Biomedical Sciences
- Physician Assistant
- Special Master’s (MBS)
-
Admissions & Financial Aid
- Tuition & Fees
-
Student Experience
-
- Student Resources by Program
- Academic & Student Support
- Wellness & Wellbeing
- Student Life
- Events & Traditions
-
-
Research
- Research Labs & Centers
- Tufts University-Tufts Medicine Research Enterprise
-
Local & Global Engagement
- Global Health Programs
- Community Engagement
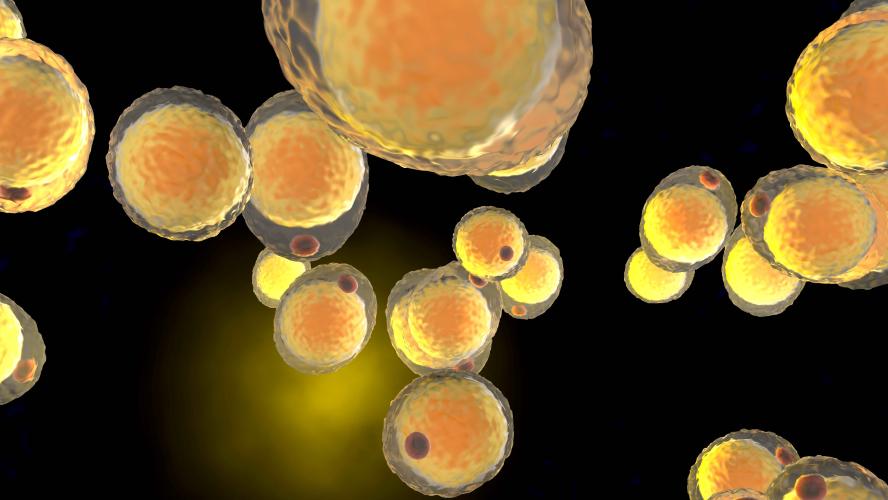
Uncovering Key Genetic Mechanisms in Fat Cell Development
Tufts scientists decode the RNA signals that decide whether fat stores or burns energy.
By Tanya Dev
For decades, fat has been viewed as public enemy number one—scapegoated by science, scorned by society, and targeted by countless trends promising to melt it away. Now, a team of biomedical researchers at Tufts University School of Medicine (TUSM) suggest we may have misunderstood our old foe. In a study published in Scientific Reports, scientists have analyzed the genetic instructions that drive fat cell development, revealing findings that could transform how we understand, treat, and even embrace fat.
Fat: Friend or Foe?
Our bodies contain two primary types of fat: white fat and brown fat. White fat acts as an energy reserve, but too much of it is associated with health risks like obesity, Type 2 diabetes, and heart disease. Brown fat, on the other hand, burns energy to generate heat and regulate body temperature, playing a protective metabolic role.
The Tufts team investigated three genetic control systems that determine whether a cell develops into white or brown fat. The idea? If scientists can tip the balance toward brown fat, we might one day turn fat into a therapeutic tool instead of a health risk.
“By encouraging the development of brown fat, we could convert fat from a metabolic liability into a therapeutic asset,” says Claire Moore, the Natalie V. Zucker Professor at TUSM and corresponding author of the study.
A Human-Centric Breakthrough
While most previous research on fat development has relied on mouse models, this study marks a shift in approach. Tufts scientists used human stem cells to track how gene activity changes as cells mature into fat cells.
“Mouse models just don’t tell the whole story,” says Moore. “There are key differences between mouse and human cells, and we wanted to map out the real playbook of fat formation in people. What we found was a coordinated network of gene regulation happening behind the scenes.”
Long Non-coding RNAs: Silent Regulators of Gene Activity
One of the study’s most exciting discoveries was a set of genetic “managers” working quietly in the background: long non-coding RNAs (lncRNAs). These molecules don’t make proteins themselves, but they help decide which genes get turned on or off—essentially influencing how fat cells develop and function.
“Some lncRNAs could nudge cells toward producing energy-storing white fat,” explains Moore. “Others could encourage the formation of brown fat, which burns calories, a critical difference in the context of metabolic health.”
The researchers identified three standout lncRNAs—LINC00312, LINC00607, and TYMSOS—that were especially active in brown fat but almost silent in white fat. That clear difference gives scientists a potential switch they can flip to help the body burn more energy and store less fat.
“These molecules could help us figure out how to turn bad fat into good fat,” Moore added. “That could be a game-changer in the fight against obesity.”
Interestingly, some of the same lncRNAs involved in fat metabolism are also linked to cancer. This suggests that the two may share common genetic factors, and that future therapies could target both at once.
Editing the Genetic Script
Tufts researchers also zoomed in on how fat cells read and edit their genetic instructions—the messages that tell them which proteins to make. They looked closely at two processes: alternative splicing and alternative polyadenylation. Both processes help cells decide how to interpret their genes, which can make a big difference in how fat cells behave.
Alternative splicing works like a film editor, allowing cells to selectively include or exclude specific gene segments so that a single gene can generate multiple versions of a protein. These variations can dramatically influence protein function, impacting key metabolic processes such as fat storage and energy expenditure, that differentiate brown fat from white fat. “If we can manipulate how fat cells splice their RNA, we may be able to encourage brown fat development—and potentially boost calorie burning,” Moore explains.
Alternative polyadenylation, another kind of genetic editing, involves trimming and modifying the tail end of RNA molecules. Think of it like adding a period, an exclamation point, or an ellipsis at the end of a sentence. These changes affect how long the message lasts, where it goes, how strongly it gets read, and whether it makes a full-length functional protein. For instance, the gene PIK3R1, which plays a critical role in regulating blood sugar, can produce a longer RNA variant through alternative polyadenylation. This extended form makes more of the complete protein, which has been shown to enhance insulin sensitivity, improving glucose uptake by cells and potentially offering protection against insulin resistance, a key characteristic of Type 2 diabetes.
Looking Ahead
As obesity and metabolic disorders continue to rise, Tufts research offers something extraordinary: a blueprint for therapies that reprogram fat cells, steering them away from storing calories and toward burning them.
By decoding the genetic systems that govern fat cell development in humans, the Tufts team has opened the door to an entirely new class of precision therapies.
“This is just the beginning,” says Moore. “We’re learning how to flip the genetic switches that shape fat—and that could unlock a whole new way to treat obesity, diabetes, and more.”
Department:
Developmental Molecular and Chemical Biology