-
About
- Departments & Offices
-
Academics
- Public Health
- Biomedical Sciences
- Physician Assistant
- Special Master’s (MBS)
-
Admissions & Financial Aid
- Tuition & Fees
-
Student Experience
-
- Student Resources by Program
- Academic & Student Support
- Wellness & Wellbeing
- Student Life
- Events & Traditions
-
-
Research
- Research Labs & Centers
- Tufts University-Tufts Medicine Research Enterprise
-
Local & Global Engagement
- Global Health Programs
- Community Engagement
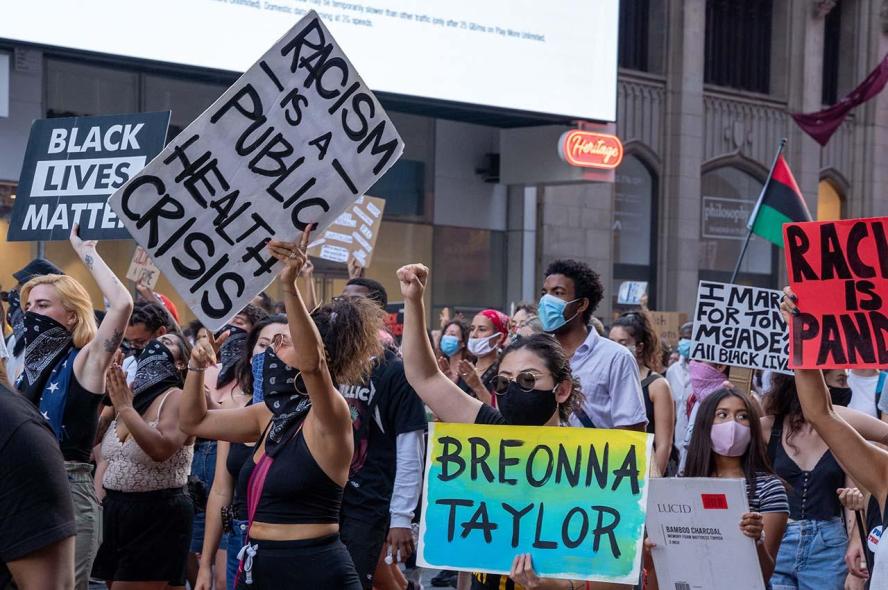
Structural Racism Is a Public Health Problem. Measuring It Can Lead to Better Solutions
A researcher quantifies racism at the state level to better understand health disparities.
Michael Siegel, a professor and researcher at Tufts University School of Medicine, has had a long career studying the public health consequences of things such as cigarettes and firearms. He didn’t intend to study structural racism. But in 2017, as Siegel tried to understand why Black people were killed in police shootings at a much higher rate than white people in some states, it was the only answer that fit the data.
“We started out with individual-level explanations, but individual differences in racial discrimination or racial bias are simply not that great across states,” says Siegel, who was a faculty member at Boston University at the time. “That’s when we started looking at the potential role of structural racism. And sure enough, when we did the analysis, it was the most significant predictor of these differences.”
That started Siegel on a research path that he is continuing at Tufts, with the goal of identifying and reducing racial health disparities, especially those associated with structural racism.
Systemic racism is a well-established public health issue. People of color in the United States are more likely to suffer worse outcomes from a variety of health conditions, including hypertension, diabetes, asthma, and heart disease because of pervasive structural biases and inequities. But in order to understand state-by-state differences, Siegel needed a way to quantify structural racism at the state level.
In 2017, Siegel and his colleagues used data from the U.S. census and national prisoner statistics to create what he believes is the first ever state racism index. It is based on five metrics: residential segregation and disparities in education, incarceration, employment, and economic status. The index rates states on a 100-point scale, with higher scores indicating more structural racism. For every 10-point increase on the scale, the researchers found a 24% increase in the disparity between Black victims and white victims in police shootings.
During the pandemic, Siegel has used this same racism index to examine disparities in COVID-19 mortality rates for Black people in the U.S. and, most recently, in vaccination rates for both Black and Latinx populations. In each case, the rates of structural racism have effectively predicted which states will have the greatest disparities between white and non-white health outcomes.
States with the worst disparities for Black people tend to be in the Northeast and upper Midwest, a fact which originally surprised Siegel but makes sense with historical context, he says. In the early 1900s, many Black Americans fled the oppressive Jim Crow South and sought new opportunities in Northern and Midwestern cities. When they arrived, they were met with hostility and often forced to live in impoverished, segregated neighborhoods. Redlining and other discriminatory practices ensured that these areas remained segregated and prevented Black Americans from gaining education and building wealth.
“It’s striking to think that things that happened a century ago, and continued over time, are producing health disparities that we observe today,” Siegel says. “These differences really do correspond to decades and decades of structural racism, and the extent of that structural racism is what explains the magnitude of the racial disparities.”
Siegel’s work demonstrates that effective public health interventions—whether they’re intended to reduce police shootings or increase vaccination rates—should target entrenched systemic inequities. He suggests investing in communities with the greatest disparities and working to remove institutional barriers to accessing health care and resources.
Today, Siegel continues to investigate the health consequences of structural racism. He is starting a project to apply the structural racism index at county- and city-levels and wants to create a publicly accessible version to help understand what measures are actually working to combat structural racism.
“You can’t evaluate how well your programs are working unless you have a measure and a baseline to compare against,” Siegel says. “We want to get this out there so that as states or cities or local governments try interventions to try to confront these problems, they’ll be able to judge their progress.”
He also plans to extend the research to include a Hispanic structural racism index in addition to a Black structural racism index.
A number of Tufts students and several local high school students will be working on these projects. Siegel hopes these new researchers will enter the field with a better understanding of effects of structural racism and the ability to look beyond individual-level explanations.
“We need to engage young people, including young people of color, in this research to help build up the cadre of future researchers who can look at these types of problems with broader societal perspectives,” Siegel says. “We need people looking for structural and institutional solutions.”
Department:
Public Health and Community Medicine