-
About
- Departments & Offices
-
Academics
- Public Health
- Biomedical Sciences
- Physician Assistant
- Special Master’s (MBS)
-
Admissions & Financial Aid
- Tuition & Fees
-
Student Experience
-
- Student Resources by Program
- Academic & Student Support
- Wellness & Wellbeing
- Student Life
- Events & Traditions
-
-
Research
- Research Labs & Centers
- Tufts University-Tufts Medicine Research Enterprise
-
Local & Global Engagement
- Pathway & Enrichment Programs
- Global Health Programs
- Community Engagement
The Home Visit
A meaningful experience for student doctors and an effective mechanism of healthcare delivery.
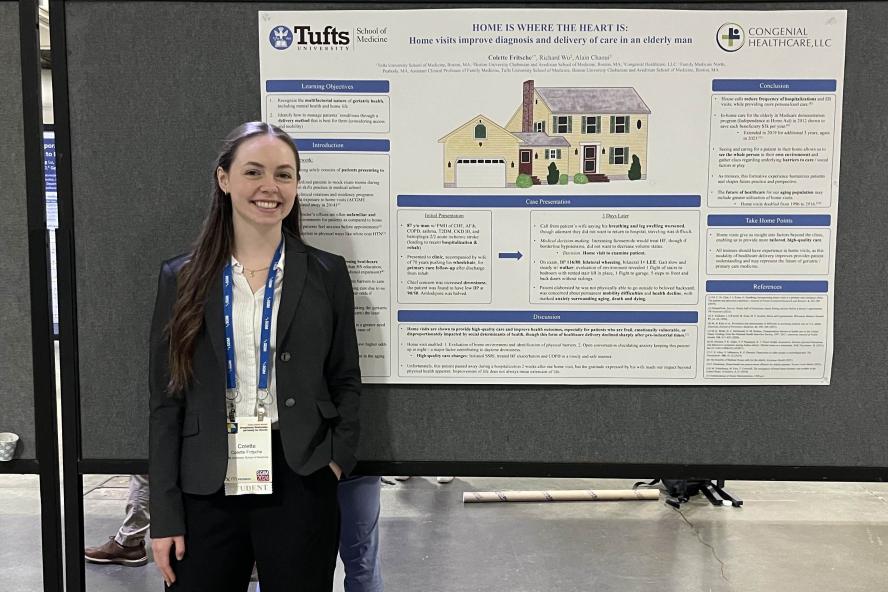
Colette Fritsche, M25
In my 3rd year of medical school, a requirement for the family medicine clerkship at Tufts University School of Medicine was to complete a home visit. To choose a patient and be welcomed into their home in order to interview them about their health and medications, understand their living environment better, and provide more holistic care initially felt unfamiliar and daunting as a student doctor. However, after having completed this experience, I understand why it is a part of the curriculum and now have begun advocating for a home visit to be a part of all medical students’ training.
The home visit enables students to experience what alternate, popular forms of healthcare delivery looked like in the past and envision how they may be revamped to provide better care to certain vulnerable populations in the future. Additionally, entering patients’ homes enables better understanding of social situations and allows for more personalized care that is not always easy in the centralized healthcare delivery system that dominates today.
My family medicine clerkship was at a small, but growing, family medicine practice in Peabody, MA. I was there with two 3rd year medical students from Boston University, who were surprised when they learned a home visit was a requirement for me. In the first week of my rotation, the need for a home visit arose. The patient was an 87-year-old gentleman who had recently been hospitalized for a stroke that left him with limited mobility, as well as heart failure exacerbations requiring increases in his diuretic regimen. He came in for a follow up appointment after being discharged from rehab and was found to have low blood pressure and increased fatigue. Three days later, his wife called saying he was experiencing increased shortness of breath and leg swelling, but they did not want to return to the hospital and traveling to the doctor would be too difficult. Because we needed to know if his blood pressure had improved prior to recommending changes to his medications, I volunteered to make a home visit. Another medical student chose to come along with me, and commented afterwards that he wished the home visit was a part of his curriculum as well.
During the home visit, we learned much more about the patient and his wife than we ever could have in the medical office. They shared their family stories with us, as well as new challenges they’d been experiencing at home with the patient’s change in physical abilities that required a walker and stairlift. We performed a physical exam and were able to recommend changes to his medications in a safe and efficient manner after discussing our findings with the doctor. Most importantly, we got to know the patient and his wife on a personal level, discussing things like end-of-life planning and the patient’s wishes. This happened in an environment that was more comfortable for them than the sterility and formality of the doctor’s office. Unfortunately, the patient passed away not long after our visit, but his wife’s gratitude was apparent even through her grief, as she thanked us over the phone for our time and care. This experience will stick with me throughout my career as one of the first times I felt like I made a true impact in the care of a patient.
Because of this formative experience, the student that accompanied me and I decided to write a narrative piece together in honor of our patient titled “The Yellow House” that has since been published in Family Medicine.1 When the opportunity arose to submit a clinical vignette for the national Society of General Internal Medicine meeting with the theme “Strengthening Relationships and Valuing Our Diversity,” I set to work.2 I researched the history and impact of home visits to back up my thoughts on how effective home visits can be. What I found was that home visits reduce the frequency of hospitalizations and ER visits, and have been shown to be cost-effective, saving each Medicare beneficiary $3k per year according to a Medicare demonstration program called the Independence at Home Act.3,4
As our population ages, home visits may represent the future of healthcare delivery for special populations such as the elderly, those with mobility difficulties and/or transportation challenges, and low-income groups. Data already shows that the number of home visits doubled between 1996 and 2016.5 Unfortunately, most medical school clinical rotations and residencies do not require home visit exposure as a part of their programs.6
The home visit shaped my perspective of the provider-patient relationship and helps humanize patients in a way that other clerkship experiences cannot. Data supports the efficacy of home visits as a means of delivering personalized healthcare and I envision their increased utilization in the years ahead. As a medical student, I’m grateful Tufts afforded me this experience and continues to include the home visit as a part of our 3rd year family medicine clerkship. I truly hope to see other medical schools in the future implementing experiences like this for the benefit of student doctors and patients alike.
1. R. Wu, C. Fritsche, A. Chaoui, The Yellow House. Family Medicine. 56, 393–393 (2024).
2. Abstracts from the 2024 Annual Meeting of the Society of General Internal Medicine. Journal of General Internal Medicine. 39, 137–1008 (2024).
3. The Benefits of Medical House Calls for the Elderly. Keystone Health (2021).
4. E. Dieckman, Home-based care proves more effective for elderly patients. Tucson Local Media (2022).
5. Independence at Home Demonstration. CMS.gov (2023).
6. M. C. St. Clair, J. J. Kram, G. Sundberg, Incorporating home visits in a primary care residency clinic: The patient and physician experience. Journal of Patient-Centered Research and Reviews. 6, 203–209 (2019).
Colette Fritsche is a fourth year MD student at Tufts University School of Medicine, where she has been involved in community outreach as the past Co-President of Tufts Chinatown Wellness Initiative and Tufts White Coats for Black Lives. She is originally from Hopkinton, MA and is applying into internal medicine residency this fall.
Department:
Family Medicine