-
About
- Departments & Offices
-
Academics
- Public Health
- Biomedical Sciences
- Physician Assistant
- Special Master’s (MBS)
-
Admissions & Financial Aid
- Tuition & Fees
-
Student Experience
-
- Student Resources by Program
- Academic & Student Support
- Wellness & Wellbeing
- Student Life
- Events & Traditions
-
-
Research
- Research Labs & Centers
- Tufts University-Tufts Medicine Research Enterprise
-
Local & Global Engagement
- Pathway & Enrichment Programs
- Global Health Programs
- Community Engagement
Summer Research Fellowship Connects Bench-to-Bedside Medicine for MD Student
Eddie Qian, M27, shares his experience studying drug resistance in melanoma cells and lessons learned about the intersection of basic and clinical research.
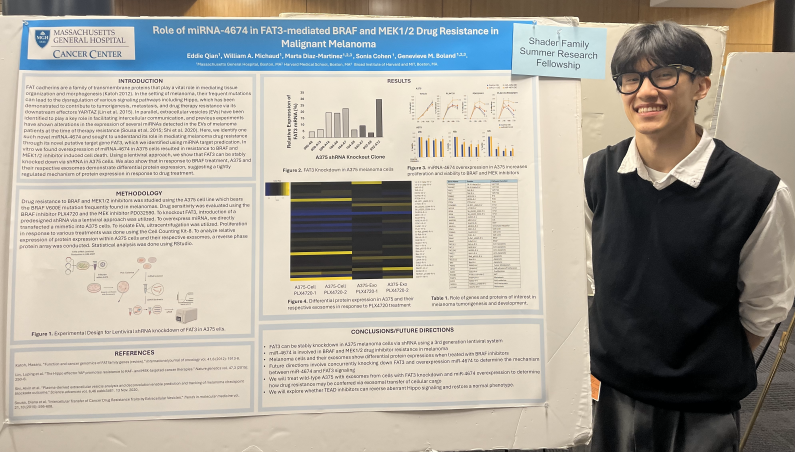
Each summer, first-year MD students at Tufts School of Medicine have the chance to immerse themselves in hands-on research, collaborating closely with faculty and research teams across various disciplines. Eddie Qian, M27, spent his summer studying how drug resistance is communicated between melanoma cells. In this Q&A, Eddie shares lessons learned and how this summer research experience shaped his future as a physician.
What was the research project you worked on, and why is it significant?
“This past summer I had the opportunity to work with Genevieve Boland, MD, PhD, at Massachusetts General Hospital, researching how drug resistance is communicated between melanoma cells. Specifically, I looked out how exosomal transfer of a novel miRNA may facilitate resistance to BRAF and MEK inhibitors by altering expression of a novel signal transducer. In simple terms, I studied how tiny packets of genetic material shared between melanoma cells might help them resist treatment. The hope is that a better understanding of the mechanisms that cause cancer to grow, spread, and resist treatment will allow us to create better therapies that can target the main drivers of melanoma development and make better clinical decisions when treating patients.”
How did you become involved in this research?
“Prior to enrolling in TUSM, I worked in two labs that focused on regenerative medicine. One revolved around finding ways to help patients recover from spinal cord injuries and the other explored alternative therapeutic strategies to promote kidney recovery following renal injury. Within both environments, I explored the novelty of stem cells and exosomes—tiny particles that cells use to communicate by sending genetic material and proteins—and grew to love understanding the pathways for pathogenesis and disease modeling. When I entered TUSM, I knew that I wanted to broaden my perspective on medicine. Given the overlap between regenerative medicine and oncology, I decided to join the Boland Lab to study exosomes through an alternative lens of disease progression and explore translational research, where benchwork directly interfaces with the clinical bedside.”
What were your primary responsibilities during your Summer Research Fellowship?
“Working in a translational research lab proved to be an eye-opening experience. On the basic research side, I conducted work in a field I was comfortable with, which included tasks such as experimental design, tissue culture, lentiviral production, and RT-qPCR. On the clinical side, I learned how to review patient charts and observed how melanoma manifested and presented within the body. I saw how melanoma samples were extracted, stored, and organized, and how collaborative partnerships facilitated data analysis. Through this experience, I grew to understand the mutual relationship between the bench and the bedside, how data and results from each side informed and built upon the other towards a common goal of treatment and cure.”
Were there any challenges you faced, and how did you overcome them? Can you describe a moment or result that was particularly rewarding or surprising?
“The biggest challenge I encountered during my research fellowship was that there was no pre-existing published work on the research I was conducting. This project became a balancing game of interpreting work that had been done and creating my own framework for where I thought the project should go. Trying to understand a little-known protein in melanoma cells proved difficult. When techniques like direct transfection—a method of introducing new genes directly into cells—did not work, I had to consider more labor-intensive options such as lentivirus (a type of virus used to deliver genetic material into cells) or CRISPR (a tool for making precise changes to DNA).
The success of the project ultimately depended on adaptability – every failure laid the groundwork for an alternative approach, every iteration evolving the trajectory of the project. The most rewarding moment was stably knocking down the FAT3 protein within melanoma cells after weeks of picking nearly 60 clones. This achievement marked the actual start of my experimental work.”
How has this experience influenced your perspective on medical research or your future career? Would you recommend this experience to other medical students?
“Central to both research and clinical practice is the idea that experiments, and treatment plans rarely pan out as intended. There is still so much we do not know about disease progression. And given that they manifest differently within each patient, careers in science require resilience and creativity to overcome challenges faced at the bench or in the clinic. This fellowship reinforced this.
I encourage other students to explore how their personal passions may intersect with medicine, whether that is through research or patient care. I believe that such a journey opens our eyes to various disparities and struggles and makes us more empathic to the realities of clinical medicine.”
Eddie Qian is a second year MD student at the Tufts University School of Medicine. Outside of research, he worked as the clinical services director of Tufts Sharewood, strengthening its community partnerships with various health institutions. He is originally from Princeton, NJ and is continuing to explore his professional interests in oncology and immunology.